The Medicaid EHR Incentive Program has ended. The information below is provided for historical purposes.
The Medicaid EHR Incentive Program was established by the HITECH Act of 2009. It was launched in October 2011 and has been officially closed out. The last year of participation was program year 2021.
The primary goal of the program was to incentivize Eligible Hospitals (EHs) and Eligible Professionals (EPs) to adopt an Electronic Health Record (EHR) system and demonstrate Meaningful Use (MU). For this purpose, the program provided financial incentives to EPs and EHs to adopt, implement, upgrade and demonstrate Meaningful Use (MU) of Certified Electronic Health Record Technology (CEHRT).
The program was administered through partnerships between CMS and the state Medicaid agencies, such as MassHealth in Massachusetts. MassHealth contracted MeHI to support and process the incentive applications in the Commonwealth. To learn more about the program, click on the section headers at the bottom of this page.
In 2018, CMS renamed the EHR Incentive Programs to the Promoting Interoperability (PI) Programs, which covers both the HITECH and MACRA MIPS programs. As such, the Medicaid EHR Incentive Program became part of the PI Programs.
Over the course of 11 years, many EPs and EHs across the Commonwealth acquired EHR systems and learned how to use their EHR to improve the quality of care. The providers also implemented electronic Health Information Exchange to more effectively share information with other providers and Patient Portals to electronically communicate with their patients.
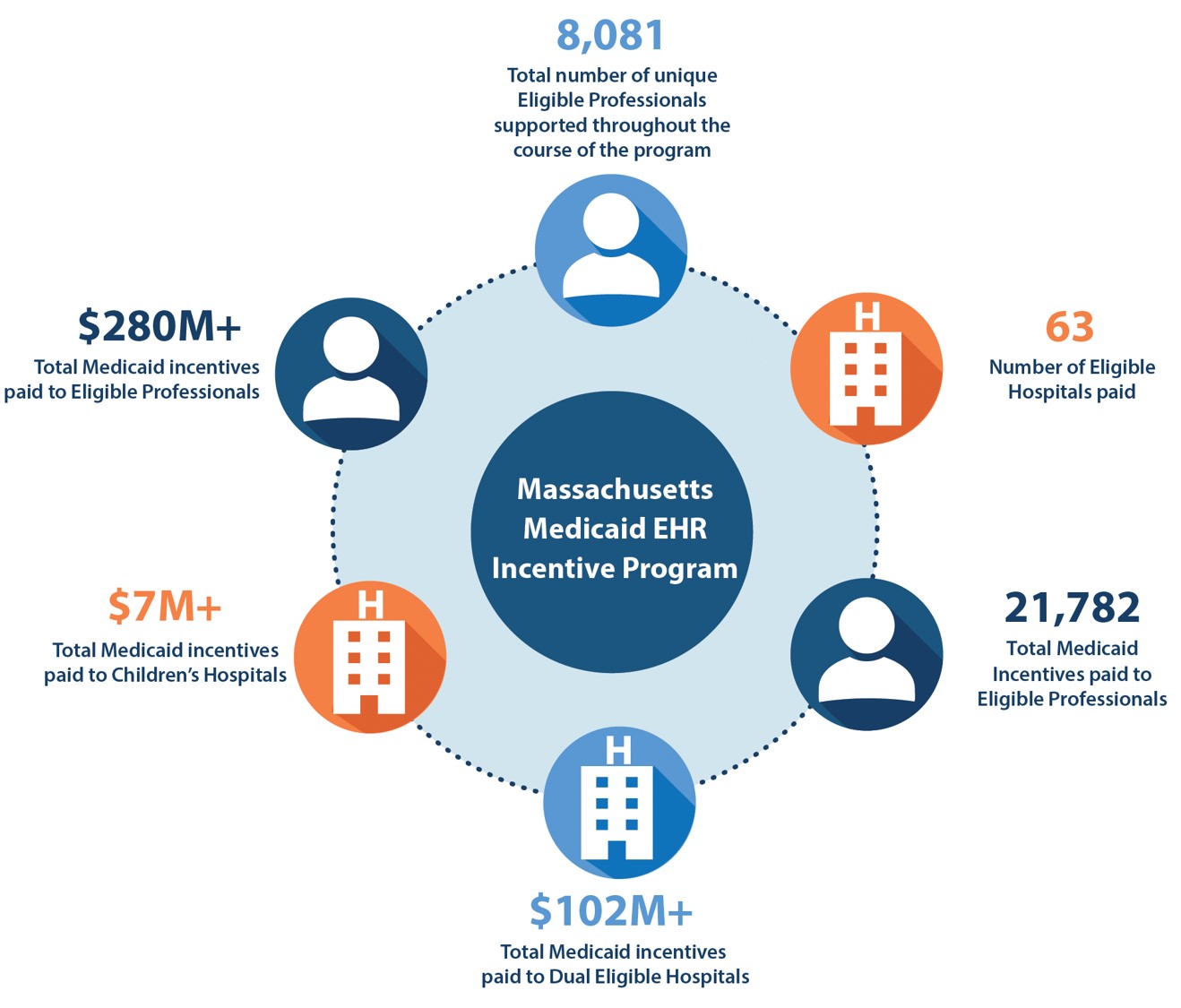
At the conclusion of this program over $280 million in incentives have been distributed to more than 8,000 unique EPs. In addition, $109 million was dispersed to 63 EHs, as shown in the graphic below. A grand total of nearly 22,000 applications were processed by MeHI under this program.
Congratulations to all the healthcare providers who successfully completed the program. Your participation significantly contributed to the increased access and advancement of care delivery in Massachusetts through the adoption of Health IT.
Select from the topics below to learn more about the requirements and history of the Medicaid EHR Incentive Program.
The program for Eligible Professionals (EPs) ended with Program Year 2021. EPs who met the eligibility criteria were able to earn up to $63,750 in financial incentives by participating in a maximum of 6 program years.
The following providers were considered Eligible Professionals (EPs) for the Medicaid EHR Incentive Program:
- Physicians (Doctors of Medicine [MD] and Doctors of Osteopathy [DO])
- Nurse Practitioners
- Psychiatric Clinical Nurse Specialists (as of program year 2016)
- Certified Nurse-Midwives
- Dentists
- Physician Assistants in a leadership position (Medical Director, CEO, or CIO)
at a Federally Qualified Health Center (FQHC) or Rural Health Clinic (RHC) - Pediatricians
When EPs worked at an Eligible Hospital (EH), both the EPs and the EH were able to apply, even if the EPs and EH used the same CEHRT.
Exclusion: EPs were considered hospital-based if 90% or more of their encounters occur at an inpatient (POS 21) or ER department (POS 23) setting. These EPs were not eligible to participate in the program, except if they contributed funds to the acquisition, implementation and maintenance of Certified EHR Technology (CEHRT) hardware and interfaces to meet Meaningful Use.
Medicaid Patient Volume
EPs had to meet a 30% Medicaid Patient Volume Threshold during a 90 day reporting period, selected from either the previous calendar year or the 12 month period leading up to their attestation date. If their Medicaid Patient Volume satisfied the threshold, the EPs could earn up to $63,750 in incentives over a 6-year period: $21,250 in the first year of participation and $8,500 in years 2 through 6. For details view this CMS presentation
Board-Certified Pediatricians could also qualify if they met a 20% threshold, but in this case the incentive was reduced to $42,500 ($14,167 year 1, and $5,667 years 2 to 6). Non-certified pediatricians had to meet the 30% threshold.
|
Medicaid Patient Volume |
= |
Number of Medicaid Patient Encounters during a 90 Day Reporting Period. |
|
Medicaid Patient Encounter |
= |
One service per day, |
|
90 Day Reporting Period |
= |
90 day consecutive period during the current calendar year, or |
FQHC/RHC Method
EPs were considered to “practice predominately” at an FQHC or RHC if 50% or more of their encounters over a 6 month period in the current calendar year occurred at an FQHC or RHC.
EPs who "practiced predominantly" at an FQHC or RHC could base their Medicaid Patient Volume on services provided to Medicaid and Needy Individuals, which includes:
- Medicaid Population (FFS);
- Medicaid 1115 Waiver Population (MCO);
- Uncompensated Care; and
- Services furnished at no cost or at a reduced cost based on the individual’s ability to pay.
Alternatively, these EPs could choose to report their volume based on the Non-FQHC/RHC Method.
Non-FQHC/RHC Method
All other EPs had to base their Medicaid Patient Volume on services to Medicaid individuals, which includes:
- Medicaid Population (FFS); and
- Medicaid 1115 Waiver Population (MCO).
In this case, CMS required that Children’s Health Insurance Program (CHIP) patients were excluded from the Medicaid Patient Volume. A CHIP reduction factor had to be applied to an EP's in-state Medicaid Patient Volume to fill this requirement. This CHIP factor varied quarterly or annually.
PVT Calculator
Failure to properly calculate PVT was the main reason why EHR Incentive applications cycled through resubmissions. To make it easier, MeHI created the PVT Calculator to automatically calculate the PVT from the EP's claims data. To learn more, select the PVT Calculator topic on this page.
A/I/U and Meaningful Use Incentives
- For the first year of participation, EPs were able to earn an incentive for Adopting, Implementing or Upgrading to CEHRT (A/I/U). The last year to participate in earning AIU incentives was Program Year 2016.
- EPs could continue to earn incentives for the Meaningful Use of CEHRT (MU). The last year to participate was Program Year 2021. As of Program Year 2017, the incentives were available only to participants who had attested and were paid A/I/U and/or MU incentives for prior Program Years.
Participation years didn't need to be consecutive as EPs could skip years, which merely delays their incentive payments.
For more details about participation and the incentive payments, read Provider FAQ fact sheet
Note: In Feb 2013, the IRS determined that the EHR incentive payments are taxable income.
Medicare versus Medicaid EHR Incentive Program
Originally, EPs could choose to participate in the Medicare EHR Incentive Program. EPs could not participate in both programs, but over the course of participation, EPs were allowed to switch once between the Medicare and Medicaid programs.
The last year to start participation in the Medicare EHR Incentive Program was 2014 and the program ended in 2016. EPs who started attesting in or before 2012, could earn up to $44,000 in financial incentives. For more details on the Medicare EHR Incentive Program visit the CMS website or view this CMS presentation
The program for Eligible Hospitals (EHs) ended with Program Year 2018. EHs that met the eligibility criteria could potentially earn millions of dollars in financial incentives.
The following hospitals were considered Eligible Hospitals (EHs) for the Medicaid EHR Incentive Program:
- Acute Care Hospitals, including Cancer and Critical Access Hospitals (CAH), where:
- Average Length of Stay (ALOS) is 25 days or less; and
- Last four digits of the CMS Certification Number (CCN) falls within 0001-0878 or 1300-1399.
- Children’s Hospitals, where:
- Last four digits of the CCN falls within 3300-3399.
Medicaid Patient Volume
To participate, Eligible Hospitals had to meet a 10% Medicaid Patient Volume Threshold over a 90 Day Reporting Period. Children's Hospitals were exempt from this threshold requirement.
|
Medicaid Patient Volume |
= |
Number of Medicaid Patient Encounters during a 90 Day Reporting Period. |
|
Medicaid Patient Encounter |
= |
One service per day, where Medicaid (FFS) or Medicaid 1115 Waiver (MCO) paid for all or part of the services. |
|
90 Day Reporting Period |
= |
90 day consecutive period during the prior federal fiscal year, which runs from Oct to Sep. EHs could choose the 90 day period they wanted to use to attest. |
CMS required that Children’s Health Insurance Program (CHIP) patients were excluded from the Medicaid Patient Volume. A CHIP reduction factor had to be applied to an EH's in-state Medicaid Patient Volume to fill this requirement. This CHIP factor varied quarterly or annually.
Eligible Hospital Incentive Calculation
The total incentive for an EH was determined based on hospital cost report data for four federal fiscal years. This could lead to millions of dollars of incentives. Read the Hospital FAQ fact sheet for the equations and an example. Use the MA Hospital Medicaid EHR Incentive Estimator (opens as MS Excel file) to determine a hospital's potential incentives.
Note: In Feb 2013, the IRS determined that the EHR incentive payments are taxable income.
Eligible Hospital Incentive Payments
Eligible Hospitals could participate for 3 years, provided they continued to meet the 10% Medicaid Patient Volume Threshold requirement. Massachusetts distributed their incentive in three annual payments.
|
Application Year |
Incentive Payment |
|---|---|
|
1 |
50% of incentive |
|
2 |
30% of incentive |
|
3 |
20% of incentive |
Medicare and Medicaid EHR Incentive Programs Dual Eligibility
All Eligible Hospitals, except Children's Hospitals, were eligible to receive incentive payments from both the Medicare and Medicaid EHR Incentive Programs in the same year. This is referred to as dually-eligible. If approved as a meaningful user of CEHRT by Medicare, an EH was automatically “deemed” a meaningful user by Medicaid. An EH had to select “Both Medicare and Medicaid” during registration to maintain this option. EHs that registered for only one program could not change their registration after a payment was initiated.
It was important for providers to assess the current state of their practice and evaluate their readiness to adhere to Meaningful Use and other program regulations. The MeHI website offered online educational resources designed to provide practical guidance and assist providers with interpreting the regulations, conducting self-assessments, and getting organized.
Meaningful Use Toolkits
In particular, the Meaningful Use Toolkits contained specific resources and tools available to assist healthcare providers to participate in the program. Originally there were two separate toolkits for EPs versus EHs. These toolkits have been merged and adapted as a historical reference for the program. To access the merged toolkit, click here.
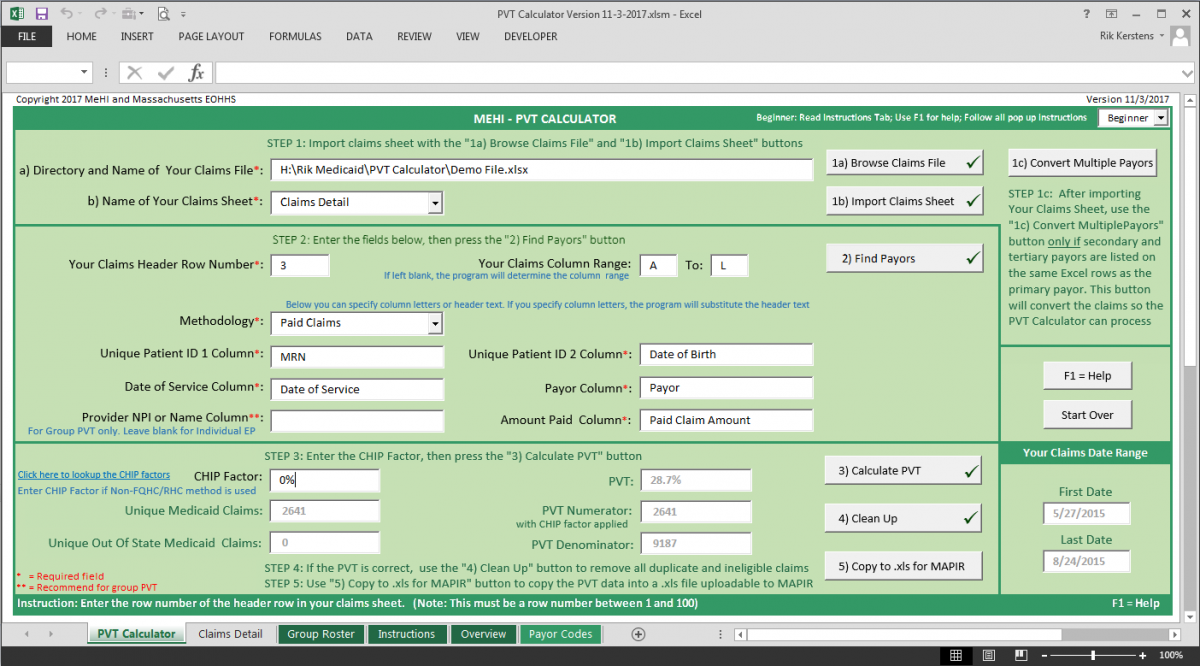
Eligible Professionals (EPs) must calculate their Medicaid Patient Volume (PVT) over a 90-day PVT Reporting Period*. Determining PVT is complex and failure to properly calculate PVT is the main reason why EHR Incentive applications cycle through resubmissions. To simplify the PVT calculation, MeHI has developed the PVT Calculator to automatically calculate the PVT from your claims data.
We recommend using the PVT Calculator to accurately calculate your PVT before attestation. The tool will enable you to upload PVT Supporting Documentation into MAPIR, when requested during the validation process. Our analysts use the PVT Calculator to validate PVT, so by using the tool you may help expedite your payment approval.
The PVT Calculator is easy to use with lots of onscreen instructions and help, see picture below. Users reported they mastered the PVT Calculator and accurately completed their PVT in 10 to 30 minutes. It is that easy, and can be used Free of Charge, so why not use it?
* The PVT Reporting Period must be, selected from either the previous calendar year or the 12 months leading up to the date of attestation.
To qualify for EHR Incentives, the PVT must meet the 30% PVT Threshold requirement (20% for Board-Certified Pediatricians).
Download PVT Calculator
The PVT Calculator contains three tools. Feature summaries are included for each tool further down this page:
• PVT Calculator: Determines the PVT based on One Claim, Per Patient, Per Day, Per EP;
• Multiple Payors Converter: Adapts an encounter-based format to the claims-based format;
• Group Roster Creator: Pre-populates the group roster with all the provider information included in the claims detail.
To download the PVT Calculator, click on the links below. The Instructions and Overview are also embedded on tabs within the PVT Calculator. Read the instructions to get started and then follow the onscreen instructions as you go.
PVT Calculator (Version 2/19/2019) - Download to use the PVT Calculator
Instructions (Version 2/19/2019) - Download to get started
Overview (Version 2/19/2019) - Download if you are interested to learn how the PVT Calculator works
Download Claims Data Templates
PVT must be calculated based on one service, per patient, per day, per EP. Health services are typically recorded as a claim and sent to Payors, like Medicaid, Managed Care Organizations, and Commercial Insurance. Claims data can serve as a proxy for the services EPs provide, and includes the information needed to determine whether an EP satisfied the required PVT eligibility threshold.
As such, the PVT Calculator determines PVT as: "Total Eligible Medicaid Claims (Numerator) divided by Total Claims (Denominator)". In this calculation, all the PVT rules are automatically applied. The PVT Calculator can handle many MS Excel and CSV claims formats, though for best practice we recommend using the claims templates below:
Individual EP - Paid Claims (Updated 5-25-17)
Individual EP - Enrollee (Paid, Zero Paid, and Denied Claims) (Updated 5-25-17)
Group - Paid Claims (Updated 5-25-17)
Group - Enrollee (Paid, Zero Paid, and Denied Claims) (Updated 5-25-17)
Feature Summary of PVT Calculator
This feature summary provides insight into what the PVT Calculator can do. Reading the summary may help you to operate the tools.
All you have to do is CLICK, and your PVT will Appear
For many EPs it will be as simple as a few CLICKS. To prepare, create your claims report, start the PVT Calculator, browse and Click to import your claims file, enter a few fields to describe your data layout, and Click to identify your Medicaid Payors. Click again to run the PVT Calculation, and voila within seconds your PVT will appear.
The PVT Calculator will identify missing data, highlight duplicate claims, and find other potential data issues. All this is done without you building complex MS Excel formulas. You will still be required to analyze the accuracy of the PVT, just as if you did the work yourself, but the PVT Calculator makes it easy for you to recognize the areas of concern.
Beginner and Expert Mode
To make it even easier, the PVT Calculator comes with Beginner and Expert modes. In Beginner mode, The PVT Calculator will guide you through the PVT process with step by step pop-up instructions. When you no longer need these instructions, you can turn them off by selecting Expert mode. In Expert mode, you will only see pop-up instructions for issues you need to address.
Individual and Group Proxy PVT Calculation
The PVT Calculator can calculate:
The PVT of an Individual EP:
• The claims data must include only the claims of the individual EP; and
• does not need to include the EP's NPI or Name.
The PVT aggregated across all providers in a Group Proxy*:
• The claims data must include the claims of all providers in the group, including the ineligible providers; and
• must include the NPI or unique Names of all eligible and ineligible providers in the group.
* When using Group Proxy, none of the EPs in the group can attest with Individual PVT. All EPs in the group must attest with the same aggregated PVT!
Paid Claims and Enrollee Methodologies
PVT Calculator lets the user select from the two available PVT calculation methodologies. Based on the chosen methodology, the PVT Calculator automatically sorts through the encounter details to determine which claims to include in the PVT Numerator and Denominator.
- Paid Claims Method:
PVT Numerator: will include all claims paid, in part or full, by Medicaid and MCOs.
PVT Denominator: will include all claims paid by Medicaid and all other payors. - Enrollee Method*:
PVT Numerator: will include all eligible Medicaid and MCO claims whether paid, or not (Zero-Paid claims).
PVT Denominator will include all claims regardless of whether these were paid.
* Using the Enrollee Methodology may increase PVT if any Medicaid services were provided for free.
Automated Identification of Medicaid Claims (Paid Claims and Enrollee Methodologies)
The PVT Calculator scans through the claims data to create a table of the Payors included in the claims data. In this Payors table, you can quickly identify the Medicaid Payors. The PVT Calculator uses the table to sort through the data to find the Medicaid claims.
Automated Identification of Eligible Zero-Paid Claims (Enrollee Methodology)
For the Enrollee Method, the PVT Calculator scans through the claims data to create a table of the Denial Reasons of Zero-Paid claims. In this Denial Reasons table, you can identify which Zero-Paid claims were ineligible for Medicaid. The PVT Calculator uses the table to automatically exclude the ineligible Zero-Paid claims.
Automated Multiple Encounter Deduping
To calculate PVT from claims data, the "one service, per patient, per day, per EP" must be interpreted to mean "one claim, per patient, per day, per EP". In other words, only one claim can be counted per day. Additional claims resulting from multiple encounters with the same patient on the same day must be excluded. PVT Calculator automatically excludes additional claims in a process called Deduping.
Automated Multiple Payor Deduping
A single patient encounter can result in claims to multiple Payors. For instance, a portion may be paid by Medicaid, while the rest is paid by a different health insurance. You can choose to use either Primary-Payor-only claims data, or Multiple-Payor claims data*.
To calculate PVT properly from Multiple-Payor claims data, only one of the claims can be counted per day. If Medicaid is one of the Multiple Payors, the Medicaid claim should be counted. PVT Calculator automatically makes this selection in the Deduping process.
* Using Multiple-Payor claims data may increase PVT if Medicaid frequently was the Secondary Payor.
FQHC/RHC, Non-FQHC and CHIP Factor Handling
EPs are considered to practice predominately at an FQHC or RHC if 50% or more of their encounters over a 6 month period in the current calendar year occur at an FQHC or RHC. These EPs can attest as FQHC/RHC or Non-FQHC EPs. All others must attest as Non-FQHC EPs.
Which claims can be included in the PVT Numerator depends on whether an EP practices predominantly at an FQHC or RHC, as shown in the table below. PVT Calculator handles FQHC/RHC EPs versus Non-FQHC EPs as follows:
-
Non-FQHC: Only Medicaid claims are counted in the PVT Numerator and the CHIP Factor* is applied to the Numerator.
- FQHC/RHC: Medicaid and Needy Individual** claims are counted in the PVT Numerator and the CHIP Factor is not applied.
* The CHIP Factor excludes an average number of Children's Health Insurance Plan encounters, as these are not eligible for EHR Incentives.
For the PVT to be calculated correctly, you have to enter the CHIP Factor applicable to the PVT Reporting Period.
** Zero-Paid Needy Individual claims need to be identified in the claims data before using the PVT Calculator, as explained in the Instructions.
|
Medicaid and Needy Individual patients to be counted in the PVT numerator |
FQHC / RHC | Non-FQHC |
|
Medicaid Population (FFS) |
YES |
YES |
|
Medicaid 1115 Waiver Population (MCO) |
YES |
YES |
|
Uncompensated Care |
YES |
NO |
|
Services furnished at no or reduced cost based on individual’s ability to pay |
YES |
NO |
|
Apply CHIP Factor to exclude Children's Health Insurance Program encounters |
NO |
YES |
Practitioner Panel PVT Calculation
The PVT Calculator can calculate the PVT of a Practitioner Panel. However, because this PVT formula is only partially based on claims data, you need to add and define the Panel Patients into the claims file, as explained in the Instructions.
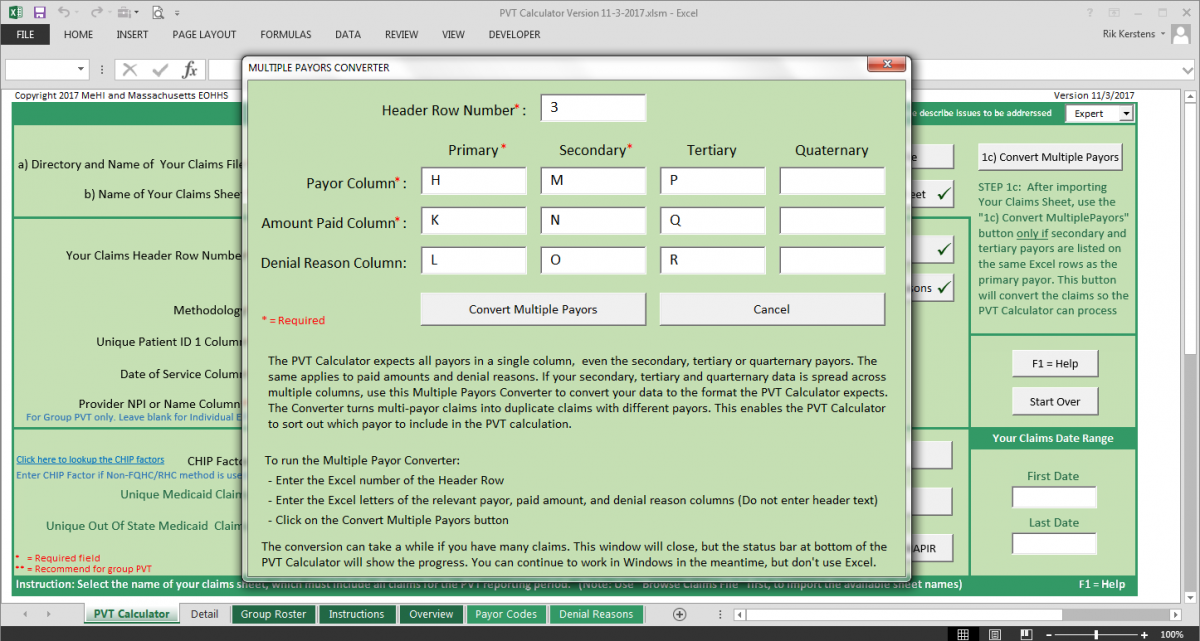
Feature Summary of Multiple Payor Converter
In the past, EPs were asked to include multiple Payors on a single row in their claims file, where each row represents a patient encounter. This is no longer necessary, because PVT Calculator's Deduper algorithm expects each Payor to be listed on a separate row.
If your claims are listed in the old format, you can use the Multiple Payors Converter tool to transform your old format into the new claims format required by the PVT Calculator. The converter can handle up to four Payor columns in the claims data, see picture below.
Feature Summary of Group Roster Creator
EPs who attest with Group Proxy PVT must submit a group roster that includes all providers included in the PVT calculation. PVT Calculator contains a tool to semi-automatically create the required roster from your claims data.
PVT Calculator highlights the roster data found in the claims data, and the missing information can be added manually, see picture below. With the click of a button, the roster can be sorted by provider Name or NPI.
Copyright Notice
The PVT Calculator program is the copyright of the Massachusetts EOHHS (Executive Office of Health and Human Services) and MeHI (Massachusetts eHealth Institute at MassTech). The program was created by MeHI, on behalf of the Massachusetts EOHHS. PVT Calculator can be downloaded for free from the MeHI website for the purpose of participation in the Medicaid EHR Incentive Program. The program cannot be redistributed for any other purpose and cannot be altered in any way without the written consent of MeHI and the Massachusetts EOHHS.
Notice of Responsibility
The PVT Calculator program is designed to enable EPs or their Designees to calculate their PVT. However, without exception, Medicaid EHR Incentive Program compliance remains the sole responsibility of the EP. The requirements are defined by CMS and MassHealth and cannot be overruled by the PVT Calculator. No claims of PVT accuracy can be made based on the results of using the PVT Calculator. The EP and Designee remain solely responsible for the accuracy of the PVT, and must verify the details and results of the PVT calculation. The EP and Designee need to make sure all data entered into PVT Calculator is correct and complete. While PVT Calculator will highlight missing or zero claims data, the EP and Designee are responsible for correcting highlighted or other data as applicable. After changing any data, the EP or Designee must rerun the PVT Calculator.
As the Medicaid EHR Incentive Program was administered as a partnership between CMS and state Medicaid agencies, registration and attestation were two separate but related processes. The program required Eligible Professionals (EPs) and Eligible Hospitals (EHs) to:
- Register for the program at the federal level using the CMS Registration & Attestation System.
- Complete annual attestations at the state level via MAPIR, the Medical Assistance Provider Incentive Repository
Registration via CMS System
To participate, an EH or EP had to first register with the CMS Registration and Attestation System (R&A) either directly or through a designee authorized to attest on their behalf. The information entered into the registration (name, address, NPI, etc) was matched against the provider's profile in the Massachusetts Medicaid Management Information System (MMIS).
If there were no discrepancies, the provider's designee received a "Welcome to MAPIR" email with instructions about how to access MAPIR, the state's attestation system.
Attestation via MAPIR System
To complete the annual attestation process, EPs and EHs in Massachusetts had to log in to MAPIR via the Provider Online Service Center on the MassHealth website, using their Virtual Gateway username and password. The MAPIR system guided participants in entering the attestation information that demonstrated that they met the program requirements:
- The first year of participation, EPs and EHs had to attest that they met the program's eligibility criteria, and demonstrate they had Adopted, Implemented, or Upgraded to (A/I/U) Certified EHR Technology (CEHRT). As of 2014, participants had the option to immediately attest to Meaningful Use in the first year, skipping A/I/U attestation.
Adopt: Acquired, purchased or secured access to CEHRT
Implement: Installed or initiated the use of CEHRT
Upgrade: Expanded the functionality to CEHRT
- In participation years 2 through 6, EPs and EHs had to attest that they still met the program's eligibility criteria, and demonstrate the Meaningful Use of CEHRT.
A list of federally Certified EHR Technology is maintained by ONC on the ONC CHPL website. In 2014 and beyond, all EPs and EHs had to submit documentation demonstrating that their EHR technology was certified according to ONC’s 2014 Edition Certification criteria, regardless of which stage of Meaningful Use they had reached.
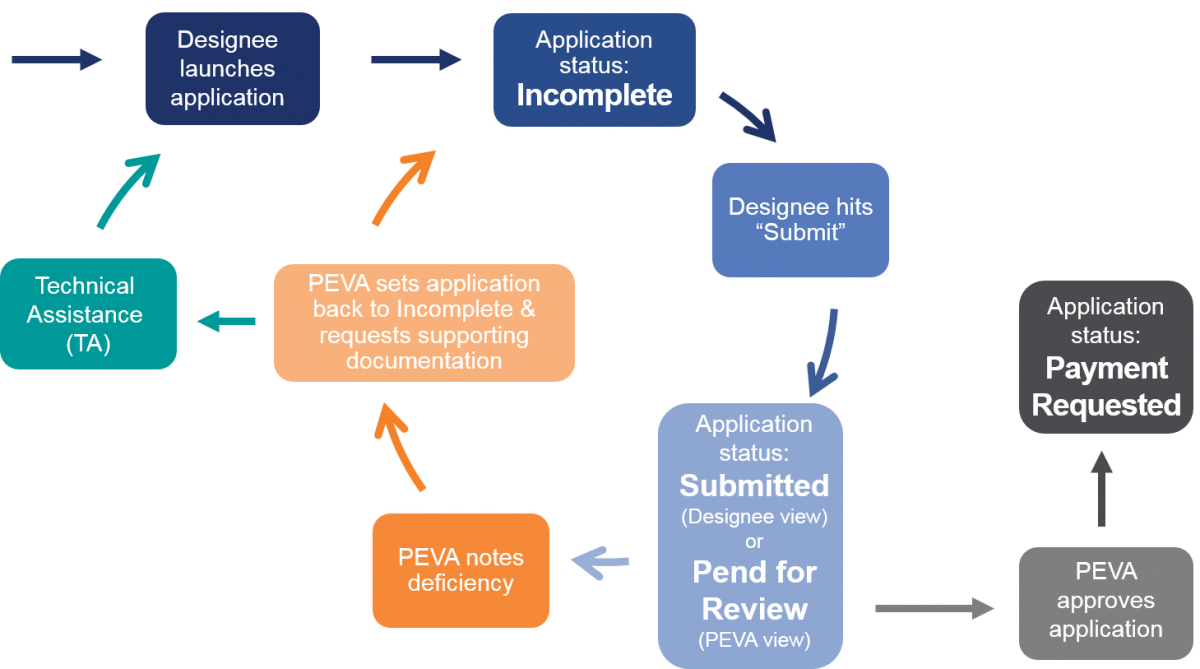
MeHI was contracted by EOHHS to validate the EHR Incentive Applications submitted by the EPs and EHs via the MAPIR application system. The Provider Enrollment and Verification Analysts (PEVAs) at MeHI validated whether the incentive applications complied with the program requirements. This included the verification that all supporting documentation properly demonstrated program eligibility and MU compliance.
Applications were allowed to go through several validation ⇒ correction ⇒ resubmission cycles before approval. At the end of a validation cycle, applications were either approved for payment, or set back to incomplete in MAPIR. When an application was set to incomplete, the provider received an email listing the discrepancies identified and the required corrections to be made. This process is shown below.
MeHI established a Technical Assistance team to guide the eligible providers in understanding the Medicaid EHR Incentive Program requirements, so they could apply for the incentives correctly and more easily. The Technical Assistance specialists were available to help providers through the Validation Process.
The Technical Assistance staff also provided educational workshops and webinars and personalized assistance via phone or WebEx. The specialists guided the providers in the Meaningful Use topics shown in the graph below.
Watch the historic webinar recordings included below to learn more about the Meaningful Use aspects of the Medicaid EHR Incentive Program. The first set includes general presentations about the program, followed by a set of presentations for specific program years in revers order of when they were presented.
General Presentations about the Program
Medicaid EHR Incentive Program Requirements - Nov 2015 - PDF
Meaningful Use Rule Changes 2015 and Beyond - Nov 2015 - PDF
Meaningful Use Public Health Reporting, Monitoring & Quality Reporting - Nov 2015 - PDF
Patient Engagement - Nov 2015 - PDF
Meaningful Use Boot Camp Webinar - Sep 2018 - PDF
Introducing the PVT Calculator - Jan 2018
Presentations ordered by Presentation Date
Program Year 2021 Meaningful Use Info Session Slides - Jun 2021
Download the slides: PDF Format
Program Year 2020 Meaningful Use Q&A Session - Jan 2021 - PDF
Timelines Program Years 2020 and 2021 - Oct 2020 - PDF
Objective 5 - Patient Electronic Access and APIs - Aug 2020 - PDF
Objective 7 - HIE - Aug 2020 - PDF
Objective 5 - API Concession Scenarios - Nov 2019 - PDF
Meaningful Use Objective 5 and API - Oct 2019 - PDF
Objective 6 - Coordination of Care - Oct 2019 - PDF
Objective 7 - Health Information Exchange - Oct 2019 - PDF
2019 Meaningful Use Info Session Slides - Sep 2019
Download the slides: PDF Format
Strategies for Patient Electronic Access and Query HIE - Sep 2019 - PDF
Clinical Decision Support for MU Stage 3 - May 2019 - PDF
API Mobile App Strategy to Meet Meaningful Use and QPP - Jan 2018
Download the slides: PDF Format
2017 Meaningful Use Overview - Oct 2017 - PDF
MU Info Session: HIE Secure Messaging Patient Portals for PY2017 - Sep 2017
Download the slides: PDF Format
Download the Q&A: PDF Format
MU Info Session: Modified Stage 2 for PY2017 - Sep 2017
Download the slides: PDF Format
Download the Q&A: PDF Format
MU Info Session: PVT Pitfalls - Sep 2017
Download the slides: PDF Format
MU Info Session: Stage 3 and ACI for PY2017 - Sep 2017
Download the slides: PDF Format
Download the Q&A: PDF Format
MU Info Session: Supporting Documents for PY2017 - Sep 2017
Download the slides: PDF Format
Download the Q&A: PDF Format
Patient Volume Threshold - Apr 2017
PCNS: How to Get Your Medicaid EHR Incentive for 2016 - Nov 2016 - PDF
Last Chance to Get Started with Medicaid EHR Incentive Program - Sep 2016 - PDF
MU Info Session - MU Objectives - Sep 2016
Download the slides: PDF Format
MU Info Session - Validation Process - Sep 2016
Download the slides: PDF Format
MU Info Session - SRA - Sep 2016
Download the slides: PDF Format
PCNS - Registration and Special Enrollment - Aug 2016 - PDF
PCNS - Patient Volume Threshold (PVT) - Aug 2016 - PDF
PCNS - Adopt, Implement, Upgrade to CEHRT - Aug 2016 - PDF
Modified Stage 2 - Attestation 101 - Jul 2016 - PDF
Modified Stage 2 - Objective #1: Protect Electronic Health Information - Jul 2016 - PDF
Modified Stage 2 - Objective #2: Clinical Decision Support - Jul 2016 - PDF
Mod Stage 2 - Obj #3: Computerized Provider Order Entry (CPOE) - Jul 2016 - PDF
Modified Stage 2 - Objective #4: Electronic Prescribing (eRx) - Jul 2016 - PDF
Modified Stage 2 - Objective #5: HIE (Summary Care Record) - Jul 2016 - PDF
Modified Stage 2 - Objective #6: Patient Specific Education - Jul 2016 - PDF
Modified Stage 2 - Objective #7: Medication Reconciliation - Jul 2016 - PDF
Modified Stage 2 - Objective #8: Patient Electronic Access - Jul 2016 - PDF
Modified Stage 2 - Objective #9: Secure Electronic Messaging - Jul 2016 - PDF
Modified Stage 2 - Objective 10: Public Health Reporting - Jul 2016 - PDF
Modified Stage 2 - Clinical Quality Measures - Jul 2016 - PDF
Meaningful Use – The Next Chapter - Jan 2016
Download the slides: PDF Format
CMS Final Rule: Stage 3 Meaningful Use and Modifications to MU for 2015-2017 - Nov 2015
Download the slides: PDF Format
Privacy & Security in Health IT - Nov 2015 - PDF
Dentists Can Achieve Meaningful Use and Receive Incentives - Jul 2015 - PDF
The Impact of Proposed Meaningful Use Rule Changes for 2015-2017 - Jun 2015 - PDF
Top Reason Why Providers Fail Meaningful Use Audits: Inadequate SRA - Mar 2015 - PDF
CMS Rule Allows Flexibility in Certified EHR Technology for 2014 - Sep 2014 - PDF
Medicaid EHR Incentive Program Updates - Sep 2014
Download the slides: PDF Format
Revisiting Patient Volume: New Strategies and Options - Dec 2013
Download the slides: PDF Format
Audit Preparation and Process Webinar - Sep 2013
Download the slides: PDF Format
Eligible Professionals Working Predominately in a Hospital Setting - Jul 2013
Download the slides: PDF Format
Patient Volume Threshold Webinar - Jul 2013
Download the slides: PDF Format
Registration and Attestation Webinar - Jun 2013
Download the slides: PDF Format
2013 Meaningful Use Deadlines & Preparing for Stage 2 - May 2013
Download the slides: PDF Format
Achieve Meaningful Use with MeHI Funding Programs - May 2013
Download the slides: PDF Format
Privacy & Security: Fundamental of SRA - Preparing for MU Measure 15 - Jan 2012
Download the slides: PDF Format