The Electronic medical record Support for Public health (ESP) project is an automated software application that analyzes electronic health record (EHR) data to identify and report conditions of interest to public health. ESP takes advantage of existing EHR data to allow clinicians to contribute detailed information to public health agencies with little or no extra work. ESP’s surveillance modules automatically execute highly accurate disease detection algorithms in order to provide meaningful surveillance without placing any extra demands upon clinicians.
Current ESP Algorithms
- Acute hepatitis A, B, and C
- Active tuberculosis
- Chlamydia
- Diabetes*, type I and II
- Giardiasis
- Gonorrhea
- Influenza like illness
- Lyme disease
- Pelvic inflammatory disease
- Pertussis
- Syphilis
*currently being validated
How ESP Works
ESP extracts details of every patient encounter every 24 hours from the primary care physician’s EHR. The ESP data model contains tables for patient demographics, vital signs, diagnosis codes, test orders, test results, medication prescriptions, allergies, social history, and provider contact details. ESP continuously searches these tables for relevant events. Target events (individual events of influenza like illness, diabetes, or other selected disease event types) are packaged into case reports and are submitted state health department electronically. In association with PopMedNet, the events can also be aggregated for population level summaries as appropriate for each surveillance target.
Making It Easier to IDENTIFY Diseases
Examples of some of ESP’s algorithms are presented in the table below. They aim to overcome the limited accuracy of diagnosis codes and the limited sensitivity of laboratory tests by integrating other information, including patients’ prescriptions, diagnoses, and test results. ESP algorithms integrate data elements across the EHR and allow detection of nuanced conditions that don’t have reliable diagnosis codes or laboratory tests such as acute hepatitis B, or type 1 versus type 2 diabetes. By reliably automating clinical analysis for selected outcomes, ESP shifts the burden of reporting from clinicians to information systems.
| CONDITION | ALGORITHM |
|---|---|
| Acute Hepatitis B |
ALT >5x normal OR AST >5x normal OR ICD9 782.4 (jaundice) AND Hepatitis B Core IgM antibody reactive within a 14 day period OR ALT >5x normal OR AST >5x normal OR ICD9 782.4 (jaundice) OR Seroconversion from hepatitis B surface antigen negative to positive within a 1 year period |
| Active Tuberculosis |
Prescription for pyrazinamide
OR Order for an AFB smear or culture AND ICD9 010.00-018.99 within the previous 14 days or following 60 days OR Prescription for ≥2 anti-tuberculous medications other than pyrazinamide |
Syndromic Surveillance
ESP includes a module that enables primary care providers to participate as sentinel surveillance sites for influenza-like illness. ESP automatically applies the Centers for Disease Control and Prevention’s (CDC) electronic definition for influenza-like illness to all patient visits each week. ESP calculates the proportion of patient visits attributable to influenza-like illness each week and stratifies the data by a variety of characteristics. These data are then sent in a weekly electronic report to the health department.
Making It Easier to REPORT Disease
Clinicians tend to underreport due to lack of knowledge of when, what and how to report cases. ESP helps primary care providers fulfill their reporting obligations by shifting the onus for reporting to electronic systems. Comparisons of ESP against conventional reporting show that ESP significantly increases the number, accuracy, completeness, and timeliness of case reports.
Calderwood MS, Platt R, Hou X, Malenfant J, Haney G, Kruskal B, et al. Real-time surveillance for tuberculosis using electronic health record data from an ambulatory practice in eastern Massachusetts. Public Health Rep 2010;125(6):843-50.
Centers for Disease Control and Prevention. Automated detection and reporting of notifiable diseases using electronic medical records versus passive surveillance--Massachusetts, June 2006-July 2007. MMWR Morb Mortal Wkly Rep 2008;57(14):373-6.
Klompas M, Haney G, Church D, Lazarus R, Hou X, Platt R. Automated identification of acute hepatitis B using electronic medical record data to facilitate public health surveillance. PLoS ONE 2008;3(7):e2626.
Klompas M, Calderwood MS, Lazarus R, Haney G, Hou X, Dumas W, et al. Automated detection of acute hepatitis C and syphilis using electronic medical record data. In: Infectious Disease Society of America Annual Meeting. Washington, D.C.; 2008.
Why Automated Reporting is Important
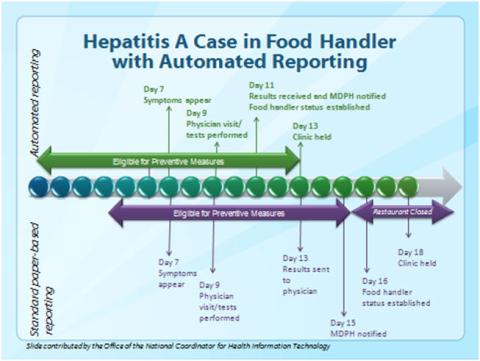
Paper-based reporting has traditionally meant delays in identifying individuals at risk and offering preventive measures which could reduce morbidity and mortality. An example of this is with acute hepatitis A infection: consider an individual who works at a popular restaurant (Bob Foodhandler) that serves approximately 100 people a day. When an individual develops hepatitis A, he is infectious (able to spread the disease) from one week before symptoms start to 2 weeks after the symptoms end. Hepatitis A is spread in a fecal-oral route, meaning if a foodhandler uses the bathroom but fails to wash his hands and then prepares food, the food could be contaminated with the hepatitis A virus and infect the person eating it.
If the health department learns that a foodhandler may have exposed some people to hepatitis A virus then they can arrange to get special prophylactic medicines for exposed people to protect them from developing hepatitis A. This has to be done very quickly, though, because the window period before the exposed person develops hepatitis A is brief. So, consider a case where Bob Foodhandler works every day before he develops symptoms and on day 7, he develops the symptoms of hepatitis A (diarrhea and jaundice, ayellowing of the eyes and skin). He continues to work while sick, but visits his physician on day 9. The physician runs a series of tests, and sends Bob Foodhandler home. Bob continues working in spite of his physician’s warning not to do so.
Bob’s doctor is required to report the case to the health department so that they can protect exposed people, but if he only sends in a paper report (the traditional method for reporting). The laboratory results do not reach the provider until day 13 and it takes an additional 2 days for the results to reach the Massachusetts Department of Public Health (MDPH). A prophylaxis clinic is arranged by MDPH, but the window of people who can receive prophylaxis has narrowed so that 400 people who were exposed to the virus are no longer able to receive preventive measures. Additionally, the window for Bob’s coworkers to receive prophylaxis has vanished so all Bob’s coworkers must be excluded from working for 28 days. As a result, the restaurant must be closed.
Now consider the benefits of electronic reporting: instead of taking 4 days for the provider to receive the laboratory results, she receives those in 2 days, and instead of MDPH being notified on day 15, they receive notification on day 11, 4 days before the paper-based model. The clinic would be offered 5 days ahead of the paper-based model, meaning all individuals at risk were eligible to receive prophylaxis and the restaurant did not need to be closed.
ESP Installation Sites
ESP is currently active in Atrius Health in Massachusetts and MetroHealth in Ohio. Atrius Health is multiprovider, multispecialty ambulatory provider system serving over 700,000 patients. MetroHealth is a mixed inpatient and ambulatory provider group with over 300,000 patients.
Additional ESP installations are underway at Berkshire Health Systems, a rural regional health information exchange, Cambridge Health Alliance and the Massachusetts League of Community Health Centers, a network of 10 community health centers that provides care for 186,000 patients from underserved populations.
